Key risk factors for Xanax addiction include being female (58% lifetime use), having a family history of substance abuse, or experiencing mental health conditions. You’re particularly vulnerable if you’re aged 50-64 or a young adult between 18-25. Physical dependency can develop within 4-6 weeks, even with prescribed use. To prevent addiction, maintain strict medication schedules, work closely with your healthcare provider, and consider non-pharmaceutical alternatives. Understanding these factors represents your first step toward safer anxiety management.
Understanding Key Demographics at Risk

Several distinct demographic patterns emerge in Xanax addiction risk, with notable variations across gender, age, and socioeconomic factors. Women face heightened vulnerability, showing stronger cravings and anxiety sensitivity than men, with 58% reporting lifetime use compared to 44% of men. This underscores the need for gender-specific interventions addressing emotional coping mechanisms.
Adults aged 50-64 demonstrate the highest prescribed use at 12.9%, while young adults (18-25) lead in misuse rates at 5.2%. White non-Hispanic adults show elevated tranquilizer misuse rates of 2.6%, though limited data on minority population access may skew these statistics. Family history and mental health comorbidities profoundly influence risk across all demographics, particularly when combined with prescription availability and poly-drug use patterns. Research shows that four in ten users develop dependency after six weeks of daily use. Patients from lower-income areas are disproportionately affected by long-term Xanax use and its associated risks. Teenagers are particularly vulnerable to addiction, with 70% of teens obtaining Xanax directly from their family’s medicine cabinet.
The Dangers of Extended Xanax Use
Extended Xanax use typically leads to physical dependency within 4-6 weeks, even when taken as prescribed, making cessation increasingly difficult without medical supervision.
Dangerous withdrawal symptoms like seizures can occur when stopping Xanax abruptly, requiring professional medical management for safe discontinuation.
For every additional 10 days of medication prescribed initially, the risk of becoming a chronic long-term user nearly doubles within the first year.
You’ll notice cognitive changes including memory problems and decreased mental processing speed, which research shows can persist even after discontinuing the medication. Regular use can impair your driving ability similar to having a blood alcohol level of 0.08%.
Your risk of serious health complications, including a 50% higher chance of hip fractures in older adults and potential links to accelerated cognitive decline, increases considerably with continued long-term use.
Physical Dependency Timeline
While many patients initially seek Xanax for short-term anxiety relief, physical dependency can develop rapidly, often within 2-4 weeks of regular use. The progression of neurological disruption follows a predictable pattern, making appropriate tapering schedules vital for safe discontinuation. Medical supervision is crucial since withdrawal can be fatal without proper care. Doctors typically prescribe short durations only to minimize dependency risks. Patients often experience severe withdrawal symptoms within 6-8 hours of their last dose.
Your physical dependency timeline typically unfolds in these stages:
- Days 1-30: Tolerance begins building, requiring increased dosage for the same effect
- Weeks 2-4: GABA receptor adaptation leads to interdose withdrawal symptoms
- Months 1-3: Complex changes in brain chemistry create persistent dependency
- Months 3+: Long-term use results in profound neuroadaptive changes, making cessation increasingly challenging
Understanding this timeline is essential for preventing severe withdrawal complications and managing expectations during the recovery process. Your healthcare provider should closely monitor these stages when developing treatment plans.
Cognitive Function Deterioration
Regular Xanax use can progressively deteriorate your cognitive functions across multiple domains, creating significant impairments in daily mental performance. The longitudinal cognitive impact manifests through compromised visuospatial abilities, executive function deficits, and significant memory impairments. You’ll notice difficulties with task planning, decision-making, and spatial reasoning.
Your neural network modifications become evident through reduced psychomotor speed and verbal learning challenges. Working memory deficits make it harder to hold and process information, while episodic memory gaps affect your ability to recall personal events. Studies reveal that up to 34 years of continuous benzodiazepine use has been documented in some patients. The brain requires increasingly higher GABA levels to maintain normal function, leading to chemical dependence.
Research shows these impairments can persist for months after stopping Xanax, with studies indicating that approximately 21% of long-term users experience deterioration across all cognitive domains. The severity of these effects correlates with duration of use and dosage levels.
Long-term Health Complications
Beyond cognitive deterioration, prolonged Xanax use inflicts extensive damage across multiple body systems, leading to severe health complications. As systemic organ damage progresses, you’ll face increasingly serious medical challenges that can become life-threatening without intervention.
Your liver and kidneys bear considerable damage, potentially leading to organ failure as toxins accumulate in your bloodstream. Daily use of Xanax can cause serious impaired judgment and decision-making abilities that persist even after stopping the medication. Users commonly experience uncontrolled muscle spasms that interfere with basic daily activities.
Neurological abnormalities emerge, including heightened seizure risk, motor impairment, and disrupted spatial orientation.
Your respiratory system becomes severely compromised, with dangerous episodes of breathing depression.
Your immune system weakens substantially, making you more vulnerable to infections and chronic illnesses.
These complications often develop gradually and may become irreversible. The risk increases extensively with continued use, especially when combined with other substances or taken in doses exceeding prescribed amounts.
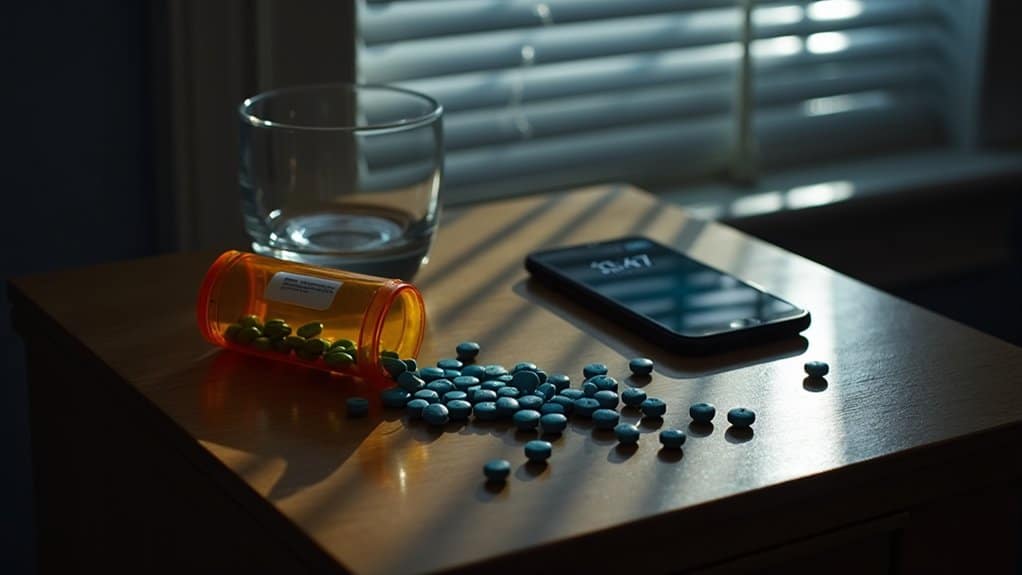
Warning Signs and High-Risk Behaviors
Early warning signs of Xanax misuse include noticeable changes in speech patterns, coordination difficulties, and unexplained mood swings that you’ll want to monitor closely. You’re at heightened risk if you find yourself frequently adjusting doses, seeking multiple prescriptions, or experiencing memory lapses during routine activities. Taking higher doses becomes necessary as tolerance builds rapidly, making dependency more likely. Physical withdrawal symptoms can appear when discontinuing use, signaling a growing dependence on the medication.
Watch for dangerous behavioral patterns such as combining Xanax with other substances, taking doses outside prescribed schedules, or engaging in risky activities while under the influence. Seeking pills from friends or family and engaging in doctor shopping behavior indicates a developing substance use disorder.
Early Behavioral Red Flags
Recognizing warning signs of Xanax addiction requires vigilant attention to five key behavioral domains: physical changes, cognitive decline, behavioral shifts, social deterioration, and loss of control. Family history patterns and lack of coping skills can accelerate these warning signs, making early detection essential.
Watch for these critical red flags:
- You’re experiencing unexplained drowsiness, slurred speech, or coordination problems during routine activities
- Your memory lapses become more frequent, especially during periods of medication use
- You’ve started neglecting responsibilities at work or home while prioritizing medication access
- You’re withdrawing from social activities and experiencing strained relationships with family members
If you notice these indicators, particularly when combined with escalating dosage needs or failed attempts to reduce use, consult a healthcare provider immediately for professional evaluation.
Dangerous Usage Patterns
The dangerous usage patterns associated with Xanax manifest through specific high-risk behaviors that markedly increase the likelihood of adverse outcomes.
You’ll face heightened addiction risks when taking immediate-release formulations at doses between 1-2mg, as these trigger stronger euphoric effects. Polypharmacy risks emerge when you combine Xanax with other substances – particularly alcohol-Xanax interactions and opioid co-use, which can lead to severe respiratory depression. Data shows one emergency visit occurs per 311 prescriptions due to such dangerous combinations.
Watch for signs of self-medicating beyond prescribed limits or using Xanax as a recreational sedative. Young adults aged 18-25 show particularly concerning patterns of high-risk combinations. Extended use without medical supervision often leads to dose escalation and dangerous withdrawal symptoms when stopped abruptly.
Critical Prevention Strategies
Implementing detailed prevention strategies remains essential for mitigating Xanax addiction risks in clinical settings. Responsible prescribing practices and extensive patient education programs form the foundation of effective prevention. Healthcare providers must maintain vigilant oversight while implementing evidence-based protocols.
Key prevention measures include:
- Strict adherence to prescription guidelines with regular patient monitoring and documented dose adjustments
- Implementation of secure medication storage protocols and proper disposal methods
- Early intervention through behavioral therapy and support group engagement when warning signs emerge
- Integration of alternative treatment approaches, including CBT and holistic practices
You’ll need to work closely with your healthcare provider to develop an individualized prevention plan that incorporates both pharmacological and non-pharmacological strategies, ensuring ideal therapeutic outcomes while minimizing addiction risks.
Building a Support Network for Recovery
Building extensive support networks considerably improves long-term recovery outcomes for individuals managing Xanax dependency. You’ll find strength in peer-led recovery groups, where shared experiences validate your journey and provide accountability. These groups range from traditional twelve-step programs to alternative approaches like SMART Recovery or Refuge Recovery.
Community-based resources offer indispensable connections through local treatment centers, cultural networks, and family support programs. You’ll benefit from structured environments that combine professional guidance with peer support, helping you develop essential coping skills and relapse prevention strategies.
When you’re facing difficult moments, 24/7 crisis hotlines provide immediate assistance and treatment referrals. Remember to engage with multiple support channels – from therapeutic relationships addressing underlying issues to family education programs that strengthen your recovery foundation.
Medical Supervision and Treatment Options

Professional medical supervision remains essential throughout Xanax discontinuation, as abrupt cessation can trigger severe withdrawal complications including seizures and psychosis. While rapid detox programs exist, evidence supports gradual stepping-down under clinical oversight for ideal outcomes.
Medically supervised tapering from Xanax prevents dangerous withdrawal effects and offers the safest path to recovery.
Key elements of medication assisted therapy include:
- Shifting to longer-acting benzodiazepines under medical supervision to facilitate safer withdrawal
- Implementing personalized tapering schedules based on your dependency level and usage history
- Utilizing non-addictive medications like SSRIs or beta-blockers to manage underlying anxiety
- Monitoring your progress through regular medical check-ups to adjust treatment protocols
Treatment facilities provide 24/7 medical oversight while managing withdrawal symptoms and addressing co-occurring mental health conditions. You’ll receive integrated care combining medical detoxification with therapeutic support for sustainable recovery outcomes.
Safe Alternatives for Anxiety Management
While prescription medications like Xanax remain common treatments for anxiety disorders, numerous evidence-based alternatives offer safer, non-addictive approaches to symptom management. Evidence-based practices demonstrate that combining holistic interventions can effectively reduce anxiety symptoms while minimizing dependency risks.
| Natural Option | Efficacy Level | Safety Profile |
|---|---|---|
| Passionflower | High | Very Safe |
| Meditation | Moderate-High | Safe |
| Yoga | Moderate-High | Safe |
| L-lysine/L-arginine | Moderate | Safe |
| Magnesium | Low-Moderate | Safe |
You’ll find the strongest clinical evidence supporting passionflower extract and mindfulness-based therapies. When implementing these alternatives, start with gradual dosing and maintain detailed symptom tracking. Consider combining herbal supplements with mindfulness practices for enhanced therapeutic benefits. Always consult healthcare providers before starting any new treatment regimen, particularly when shifting from prescription medications.
Frequently Asked Questions
Can I Still Drive or Operate Machinery While Taking Prescribed Xanax?
You shouldn’t drive or operate machinery while taking Xanax, even with a valid prescription. The medication greatly affects your cognitive abilities, causing delayed reaction times and impaired judgment.
Workplace safety concerns make this especially critical when handling equipment. Research shows that benzodiazepines like Xanax increase accident risks by up to 8.5 times.
You’ll need to discuss alternative transportation options with your healthcare provider during treatment periods.
How Long Does Xanax Withdrawal Typically Last After Stopping Use?
The duration of Xanax withdrawal typically lasts 1-4 weeks, but you’ll experience varying severity of withdrawal symptoms throughout this period. You’ll notice initial symptoms within 6-12 hours after your last dose, with peak intensity occurring around days 2-5.
The severity of withdrawal depends on your usage history and tapering approach. It’s essential that you don’t stop taking Xanax abruptly always withdraw under medical supervision to manage potentially dangerous symptoms safely.
Will Insurance Cover Xanax Addiction Treatment and Rehabilitation Programs?
Most insurance plans will cover your Xanax addiction treatment and rehabilitation programs, thanks to ACA requirements and parity laws. You’ll need to verify your specific medication coverage options and treatment program costs with your provider.
Marketplace plans, Medicare, and Medicaid typically include both inpatient and outpatient services, though you may need pre-authorization. Remember that out-of-pocket expenses like copays and deductibles will vary depending on your plan’s structure.
Can Genetic Factors Influence My Likelihood of Developing Xanax Dependency?
Yes, your genetic makeup can substantially influence your risk of developing Xanax dependency. If you have a family history of substance abuse or anxiety disorders, you’re more likely to experience addiction due to inherited biological predisposition.
Your genes affect how your brain processes Xanax, particularly through GABA receptor interactions and neurotransmitter systems. This genetic vulnerability doesn’t guarantee addiction but does mean you’ll need extra caution when using benzodiazepines.
What’s the Success Rate for People Recovering From Xanax Addiction?
You’ll be encouraged to know that about 75% of people recover successfully from Xanax addiction, especially when following detailed treatment plans.
Your chances improve considerably with medication-assisted treatment to manage withdrawal symptoms and relapse prevention strategies. While recovery can be challenging, statistics show that 70% of patients report better outcomes within their first year of treatment when they stick to structured programs and ongoing support services.






